October is an important awareness month highlighting ADHD and OCD, two mental health disorders that unfortunately still carry a lot of stigmas, mainly because they are misunderstood among the general population.
Obsessive-compulsive disorder (OCD) and attention-deficit hyperactivity disorder (ADHD) are common mental health disorders. To the untrained eye, some of the symptoms associated with attention and concentration can appear similar, especially in children and adolescents. As a result, these disorders are often confused with one another, even though they are strikingly different in clinical presentation and treatment.
However, the comorbidity of ADHD and OCD is more common than one may think, meaning that individuals with OCD have up to 30% likelihood of developing ADHD. Comorbid OCD and ADHD enhance the symptoms of each other, and OCD also has an earlier onset when ADHD is present.
ADHD
ADHD is characterized by impulsivity, hyperactivity, distractibility, and difficulty following instructions and completing tasks.
Individuals diagnosed with ADHD could have either inattentive or hyperactive-impulsive presentation or both. The presentations are:
- Attention-deficit/hyperactivity: combined presentation
- Attention-deficit/hyperactivity: predominantly inattentive presentation
- Attention-deficit/hyperactivity: predominantly hyperactive-impulsive presentation
ADHD is considered an externalizing disorder, affecting how people outwardly relate to their environment. Individuals with ADHD may exhibit inattention, lack of impulse control, and risky behaviors.
Symptoms of ADHD include the following:
- Easily distracted/short attention span
- Starting new tasks before completing old ones
- Losing things
- Forgetting things
- Poor organizational skills
- Inability to focus or follow directions
- Poor listening skills
- Speaking out of turn/interrupting conversations
- Inability to sit still
- Taking risks in activities without any regard for personal safety
- Mood swings/irritability
- Fidgeting
- Impatient
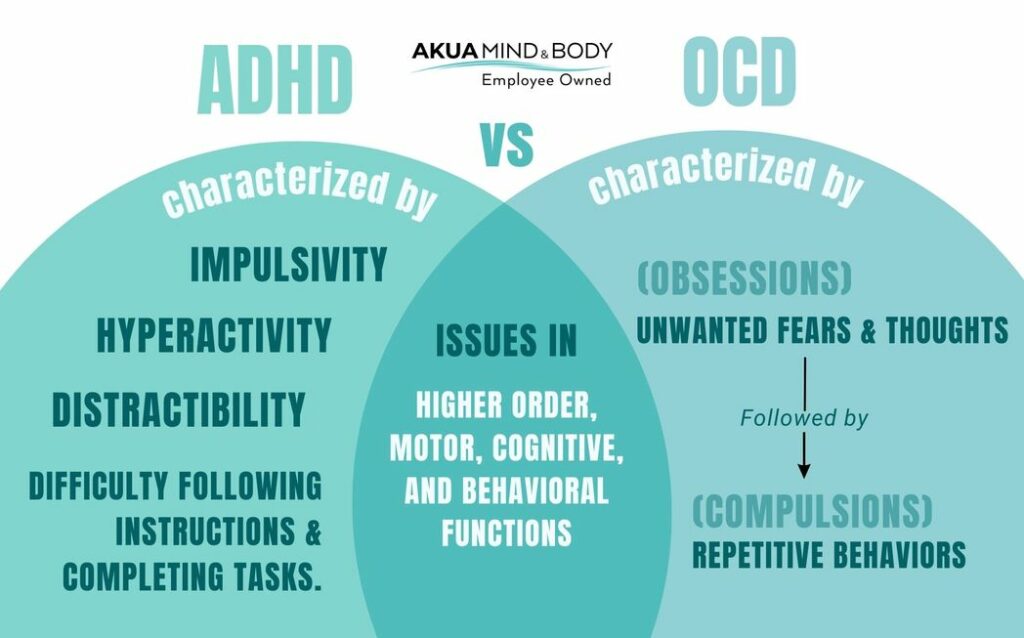
Shared brain regions
Although ADHD and OCD are separate mental health disorders with differing symptoms and treatment modalities, there is some overlap between these two disorders. Both disorders affect the frontostriatal portion of the brain, an area responsible for higher order, motor, cognitive, and behavioral functions. Frontal-striatal systems are anatomically defined circuits connecting frontal cortical areas to corresponding locations in the striatum (basal ganglia). However, individuals with ADHD exhibit decreased activity in the frontostriatal circuits, and individuals with OCD exhibit significantly increased activity in this region.
Obsessive-compulsive disorder
Obsessive-compulsive disorder (OCD) is a mental health disorder characterized by unwanted fears and thoughts (obsessions) followed by repetitive behaviors (compulsions) to relieve the unwanted thoughts. Some examples of distressing obsessions in individuals with OCD include doubts about leaving the stove on, locking the door, fear of uncleanliness or being contaminated by objects, and severe stress when things are not organized in a specific way. These obsessive thoughts are distressing and, therefore, are often carried out by compulsive actions to relieve the distress.
Some common examples of compulsions include counting, unlocking, locking the door, turning the stove on and off, and repetitively organizing, cleaning, or checking. OCD is not considered an anxiety disorder, as worry and obsessions are very different. As a result, OCD is no longer classified as an anxiety disorder in the DSM, but it is classified under Obsessive-Compulsive and Related Disorders. Many individuals with OCD have extreme anxiety about their unwanted thoughts, but it is essential to remember that worries are not the same as obsessions. To qualify as having obsessions in OCD, an individual must have recurrent and persistent thoughts, urges, or impulses that cause distress and are experienced as intrusive and unwanted.
OCD is characterized as an internalizing disorder, meaning individuals with OCD respond to anxiety-producing environments by turning inward. People with OCD tend to demonstrate a more inhibited temperament and avoid risky or potentially harmful situations. They are generally overly concerned with their actions’ consequences and tend not to act impulsively.
Impulsivity vs. compulsivity
Impulsivity is characterized by the inability to resist impulses and urges, delaying gratification deficits, unreflective decision-making, and premature behavior. Compulsivity is characterized by perseverative and repetitive action and is ruminative and rigid. These constructs co-occur in separate cases of ADHD and OCD at varying severities.
Treatment for ADHD vs. treatment for OCD
The combination of medication and cognitive behavioral therapy has proven beneficial in treating OCD and ADHD. However, medications and types of CBT differ for each disorder. The effectiveness of selective serotonin reuptake inhibitors (SSRIs) in treating OCD has been well established. The psychotherapy of choice for the treatment of OCD is exposure and response prevention (ERP), which is a form of cognitive behavioral therapy. In ERP therapy, people with OCD are placed in situations where they are gradually exposed to their obsessions and asked not to perform the compulsions that usually ease their anxiety and distress.
The first line of treatment for ADHD has been methylphenidate or dexamphetamine, both prescription stimulants. Cognitive behavior therapy tailored for ADHD behaviors has been shown to improve academic and organizational skills, problem-solving and prioritizing tasks, and manage unhelpful thinking and behavioral patterns.